Human Mobility, Epidemiology, and Health Disparity
During the COVID-19 pandemic, non-pharmaceutical interventions were widely employed to contain the dissemination of the virus by restricting people’s travel and physical contact. I focus on building integrated econometric, epidemiological, and simulation models to examine (causal) relations among human mobility, public policies, vaccination, and virus transmission, controlling for confounding effects from socioeconomic conditions. In the future, I intend to extend my research to a broad scope of health scenarios such as SARS-Cov-2 variants, AIDS, and influenza.
Human Mobility, Infectious Disease, and Health Disparity 😷 😷 😷 🏃🏃🏃
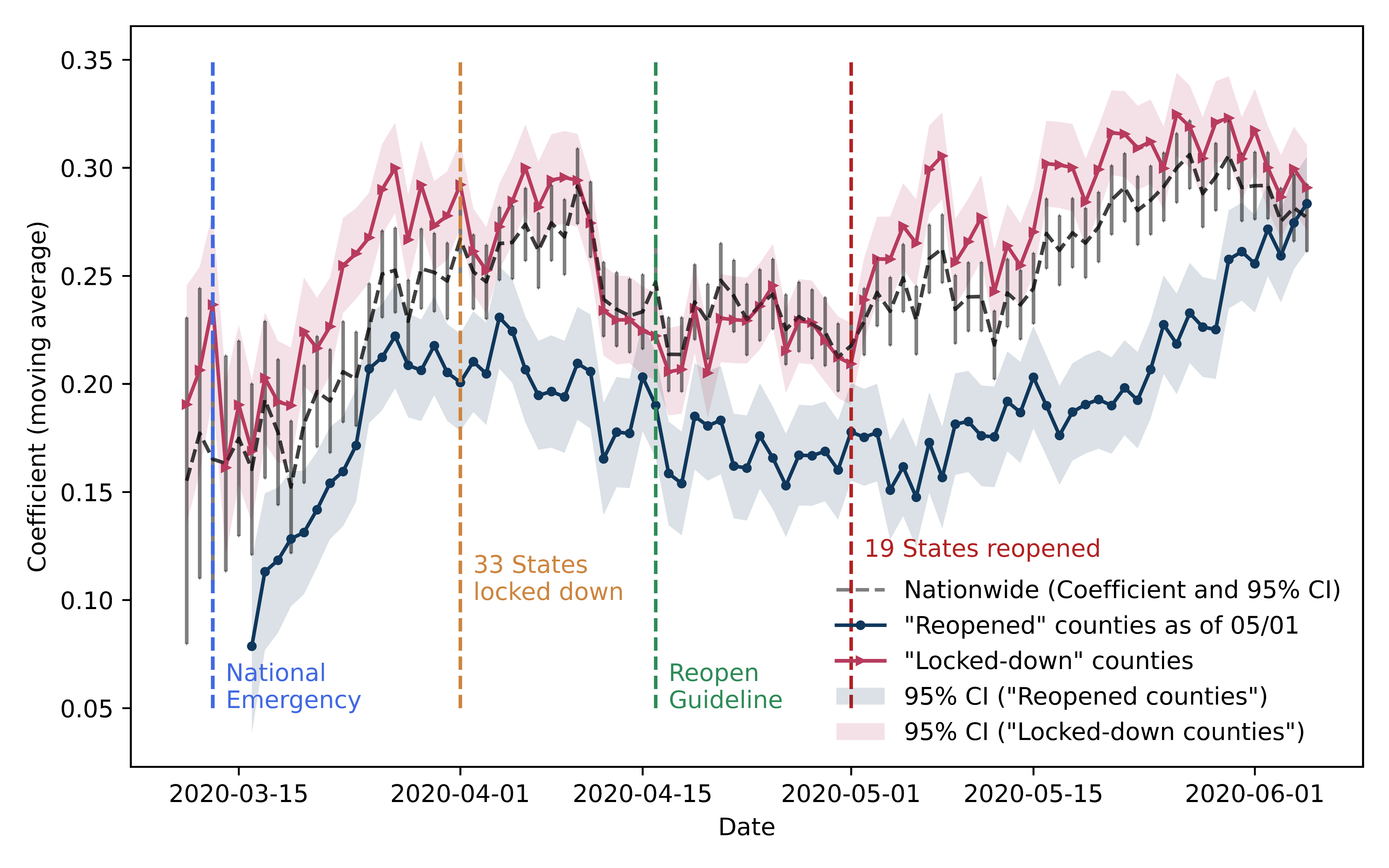
[PNAS] At the beginning of COVID-19 pandemic, we quantify the change of mobility inflow across the nation and statistically model the time-varying relationship between inflow and the infections. Our analysis highlights the dynamics in a positive relationship between mobility inflow and the number of infections during the COVID-19 onset. This relationship is found to be much stronger in partially reopened regions.
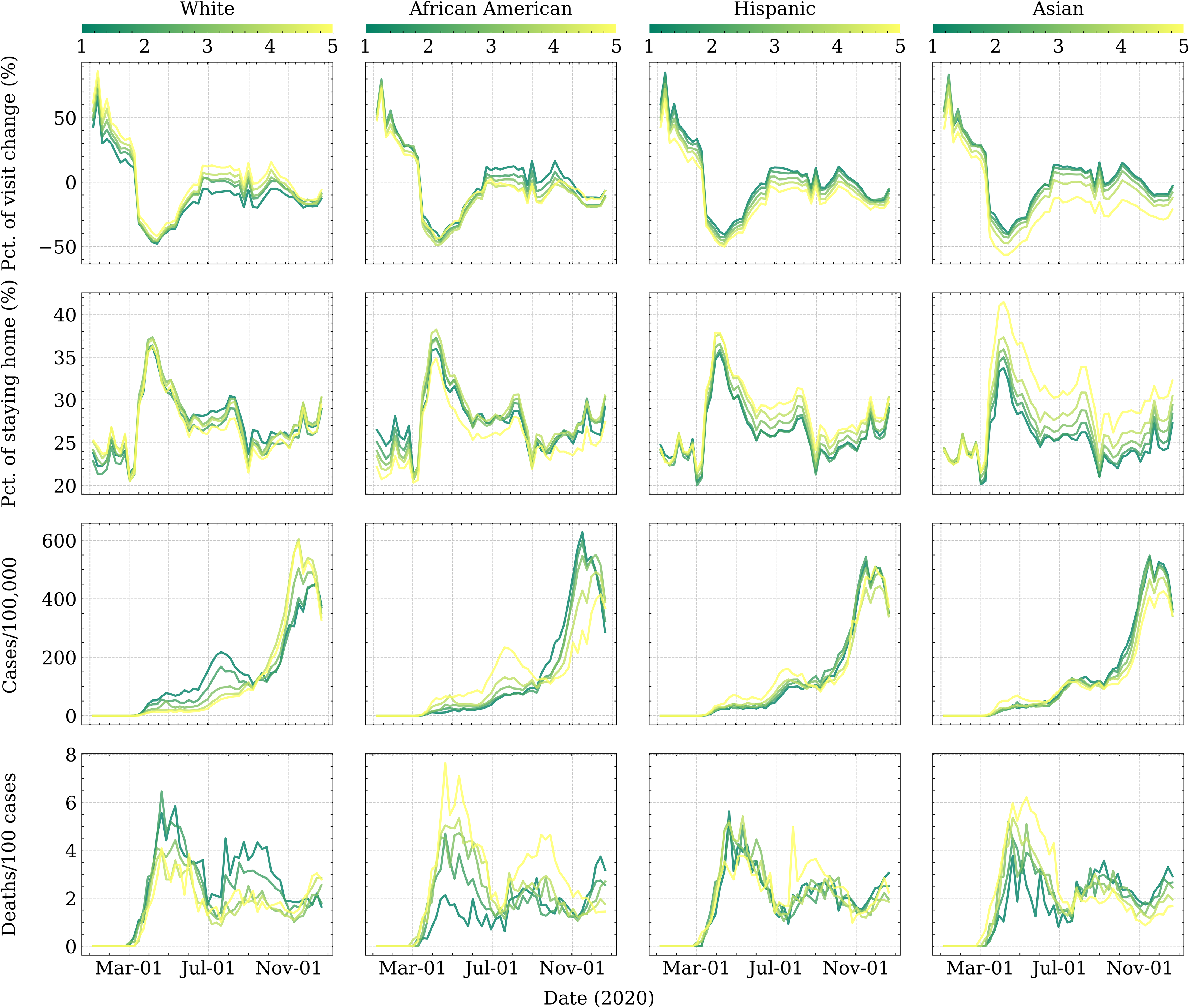
[SCS] We focus on seeking the socioeconomic roots of health disparities in COVID-19 pandemic by exploring the relationships between COVID-19 outcomes and other exogenous factors, including socioeconomics, demographics, occupation, and partisanship. We find salient structural inequality: Social distancing is a “privilege” for advantaged socioeconomic groups, while disadvantaged groups consistently bear a larger brunt of case and death tolls, regardless of high vaccination rates.
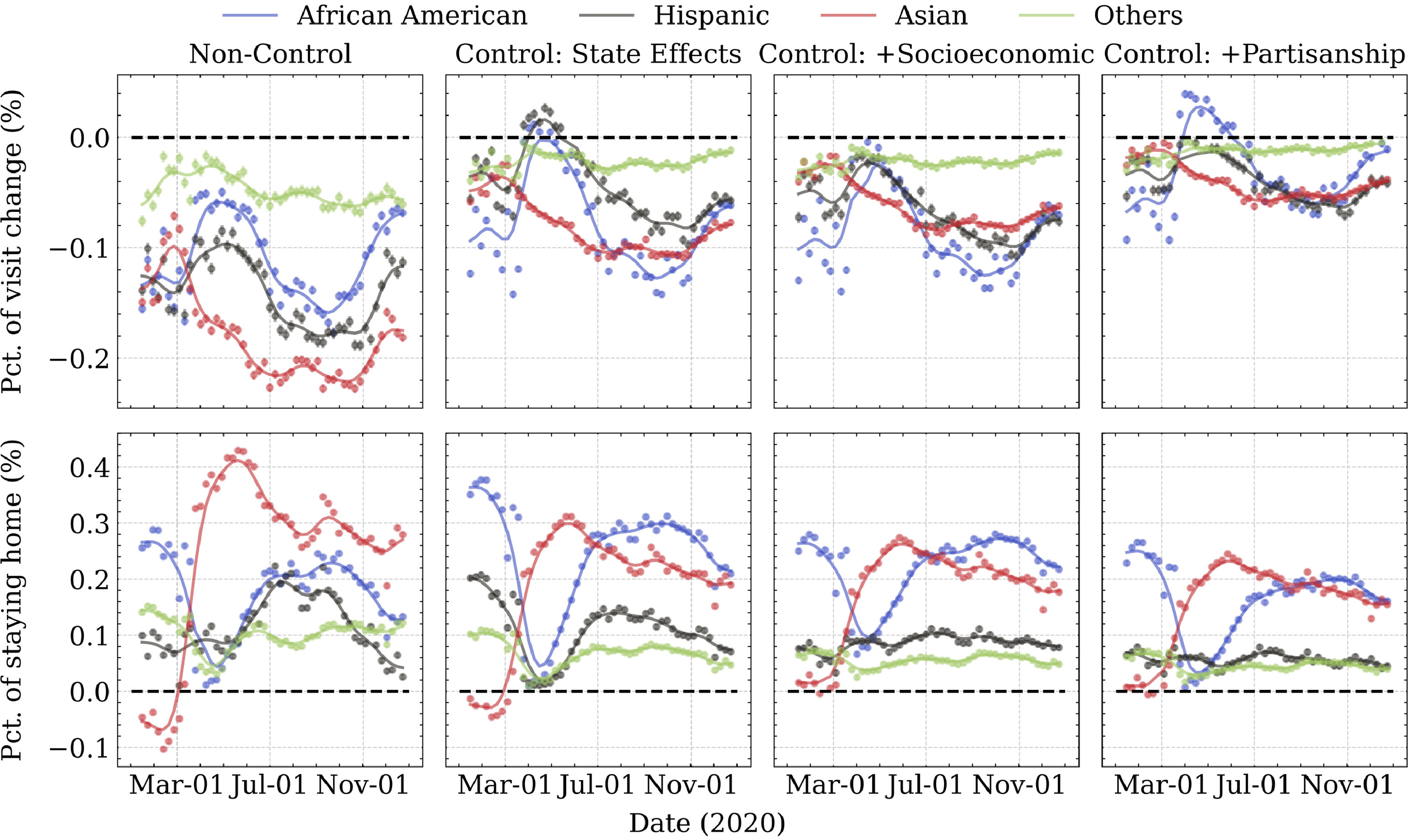
[PLOS] We jointly examined county-level racial/ethnic differences in compliance with stay-at-home orders and COVID-19 health outcomes during 2020, leveraging two-year geo-tracking data of mobile devices across ~4.4 million POIs in the contiguous US. Through a set of structural equation modeling, we quantified how racial/ethnic differences in following stay-at-home orders could mediate COVID-19 health outcomes. Mediation analyses revealed that human mobility only statistically influenced infection rate but not case-fatality ratio, and such mediation effects varied substantially among racial/ethnic compositions.
Human Mobility and Vaccination 💉💉💉🏃🏃🏃
[Vaccine] Vaccine hesitancy has been identified as a major obstacle preventing comprehensive immunization coverage. Our study examines whether the prospective vaccine hesitancy eventually translates into differential vaccination rates. Mediation analysis demonstrates that COVID-19 vaccine hesitancy cannot fully explain disparities in vaccination coverage across the contiguous US, challenging the popular narrative that portrays vaccine hesitancy as a root cause of disparities in vaccination.
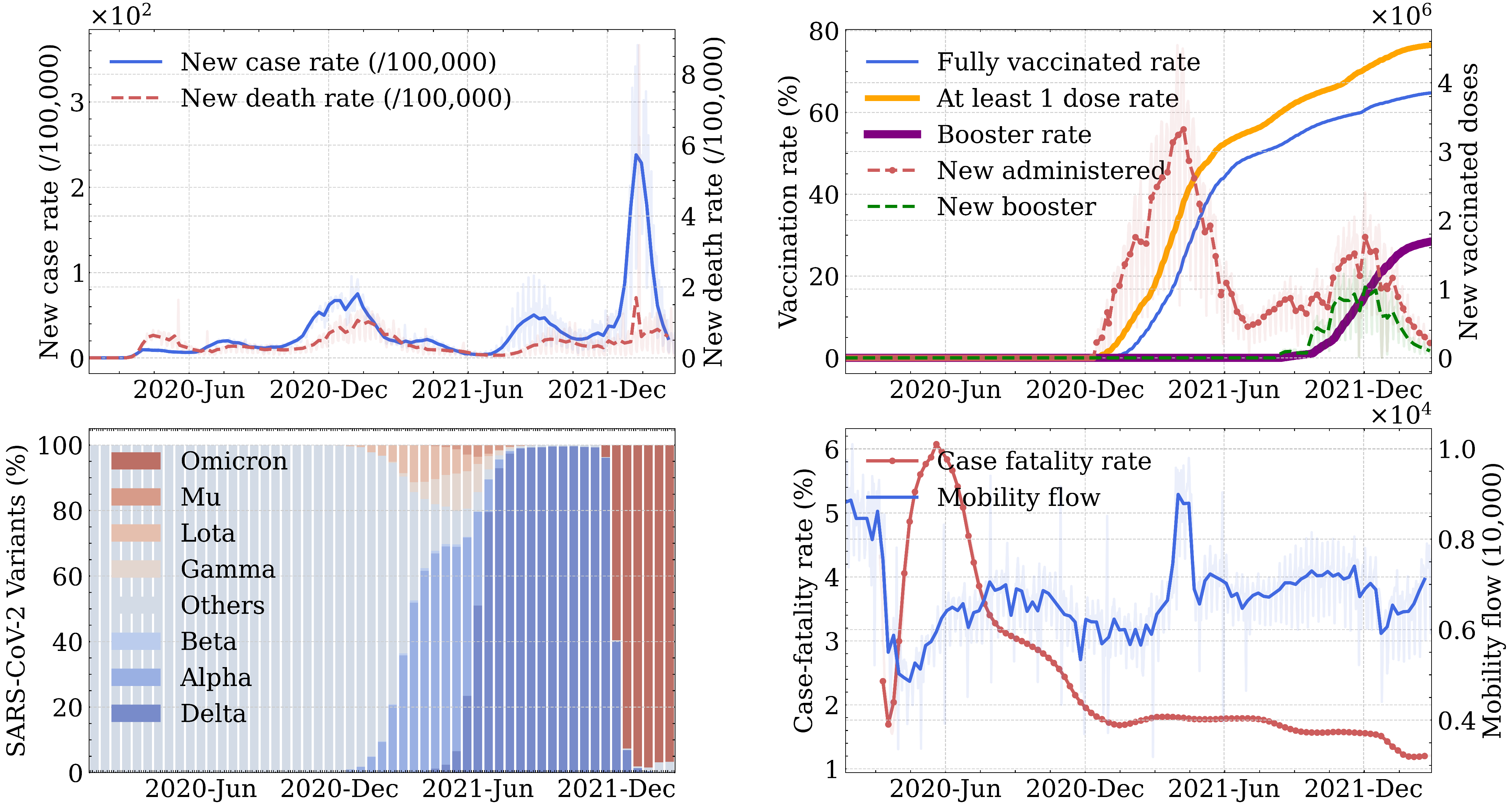
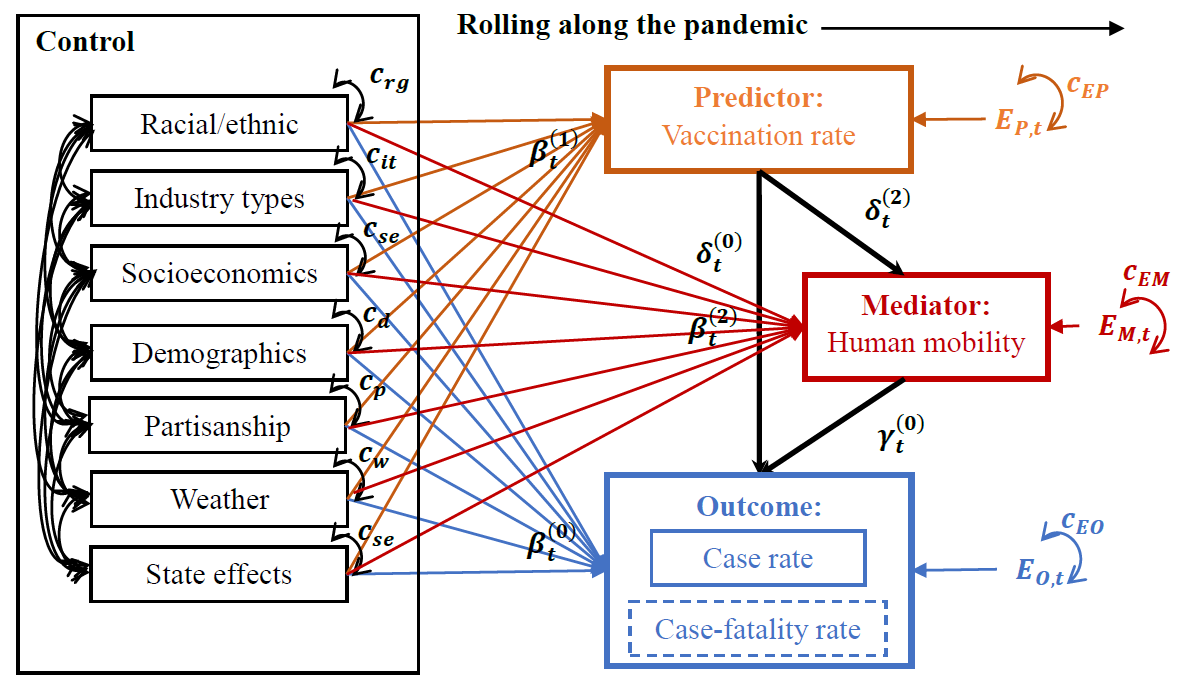
[Vaccine] Leveraging over two years of county-level US data, we investigate relationships among vaccination, human mobility, and COVID-19 health outcomes. Results show that vaccine effectiveness against case rate lost significance during the Omicron surge, while its effectiveness against case-fatality rate remained significant. My work has gained interest from NIH in sponsoring its further development into an agent-based human mobility and epidemiology model to forecast future infection spatiotemporal dynamics.